Abortion Info
In accordance with Iowa’s current laws, abortion is available up to the detection of cardiac activity, with exceptions as permitted under state law. The Emma Goldman Clinic offers procedural and medication abortion services within that timeframe.
We believe every person has the fundamental right to determine the outcome of their pregnancy—regardless of age, marital status, race, gender identity, or income. Our commitment to reproductive justice guides everything we do, and we will continue to provide care, support, and advocacy in the face of unjust restrictions.
If You Think You Are Pregnant
If you think you may be pregnant, get a pregnancy test if you have any of the following symptoms: a missed menstrual period, swollen or tender breasts, nausea, vomiting, appetite changes, frequent urination, fatigue, dizziness, or feeling bloated. Urine tests can be done by our clinic, your doctor, a family planning facility, or by using a do-it-yourself home test purchased from your local pharmacy. It may be preferable, as well as less expensive, to visit a health center. There, in addition to receiving your test results, you can usually get advice on pregnancy, birth control, or other health problems that might be causing your symptoms. An accurate test is best achieved on a specimen from the first urination of the day.
Urine tests vary in sensitivity, with some able to detect pregnancy as early as 10 days after conception. If you get a negative test but continue to have symptoms listed above, continue to get tested every two weeks and see a doctor if you have missed two periods. If you get a positive test, it is usually a good idea to get a pelvic examination if you have any doubt about the date or normality of your last period. This will give you fairly accurate information on how far along the pregnancy has progressed and how much time you have to consider your options.
Why Me?
Nature conspires to perpetuate the species. Sexual intimacy is a strong emotional and physical need. Even the best contraceptives, the staunchest moral sermons, and the most reasonable couple cannot always stop Nature from doing her job. Over one million unplanned pregnancies occur every year in this country.
Sometimes birth control fails. Sometimes access to sexual information and birth control devices is a problem, particularly for teenagers and those who are poor or live in rural areas. Sometimes individuals get confused by mixed social messages about sexuality. For example, on one hand we are bombarded with images of eroticism in advertising, movies, and music. On the other hand we hear messages from our earliest cultural influences, such as parents, teachers, and religious leaders, about how sex should be used for procreation.
These conflicting messages sometimes translate into inconsistent birth control activity. These are just some of the reasons why pregnancy occurs when it is not wanted. However, knowing reasons does not always help lessen the sense of unfairness or the shock and conflict felt upon learning that you are pregnant.
Medical Disclaimer
The information provided on the Emma Goldman Clinic website is for general educational and informational purposes only and is not intended as medical advice, diagnosis, or treatment. This content should not be used as a substitute for professional medical care from a qualified health care provider who is familiar with your individual health needs.
Always seek the advice of your physician, nurse practitioner, or other qualified health care provider regarding any questions you may have about a medical condition, treatment, or health goals. Do not disregard or delay seeking professional medical advice because of something you have read on this site.
If you have questions regarding care you received at the Emma Goldman clinic, please call us at 319-337-2111. If you feel as though you are experiencing a medical emergency, please call 911.
Links to external websites are provided for convenience and informational purposes only; the Emma Goldman Clinic is not responsible for the content, accuracy, or privacy practices of those sites.
Use of this website does not establish a patient–provider relationship with the Emma Goldman Clinic.
Disclaimer: Information on this site is for education only and is not medical advice. Always consult a qualified health care provider about your personal health needs. In an emergency, call 911. Use of this site does not create a patient–provider relationship.
Making A Decision
Sorting Through Conflicting Feelings
Pregnancy can bring up a wide range of emotions. These feelings may shift from moment to moment and are shaped by many factors—such as your personality, age, life circumstances, and relationships. It’s normal to feel conflicted.
Some people may feel reassured to learn they are fertile, yet unsettled by the timing. Others may feel heartened by the symbol of love and commitment that pregnancy can represent, while also feeling stressed or unprepared for the challenges it may bring. You may wonder about the future—about a potential child’s health, identity, or how pregnancy could impact your life.
It’s also common to experience difficult emotions:
- Fear of how pregnancy may change your relationships or daily life
- Guilt or shame, sometimes tied to how abortion or pregnancy is perceived in families, communities, or faith traditions
- Anger at partners, parents, or society for limiting access to birth control or information
- Anxiety about medical procedures, pain, or uncertainty about the outcome
- Complex grief and trauma if a pregnancy results from sexual violence
Every person’s feelings are unique, valid, and worthy of care.
Living with Ambivalence
Ambivalence—feeling pulled in different directions at once—is very common. What matters most is giving yourself the time and space to sort through your feelings before deciding whether to continue or end a pregnancy.
Seeking Support
It can help to talk with a trusted, nonjudgmental listener. This might be:
- A close friend or relative
- A faith or spiritual leader
- A trained counselor or healthcare provider
Choose someone who has your best interests at heart, can listen without judgment, and won’t pressure you toward any particular decision.
You may also want to talk openly with people who are part of your life and your pregnancy—such as a partner, co-parent, or family members.
Exploring Options
Consider all possibilities, including:
- Continuing the pregnancy and parenting
- Continuing the pregnancy and making an adoption plan
- Ending the pregnancy with abortion care
Seeking accurate, unbiased information is key. Social service organizations, healthcare providers, and clinics like Emma Goldman can offer factual details about medical options, emotional support, and financial resources.
Making a simple list of pros and cons for each option can sometimes help clarify your priorities. Remember, this decision is yours—and caring for both your heart and your health matters most.
Making an Abortion Appointment
Call us at (319) 337-2111 or 1 (800) 848-7684
The person who answers the phone will make your appointment, give you instructions, and explain the costs involved.
Ask about medical insurance coverage. If you are under the age of 18, ask about parental notification requirements. Payment in full is required at the time of the appointment. The Emma Goldman Clinic has a subsidy program that depends on your annual household income and your access to insurance and Medicaid. Call us to find out how our subsidized fee program can work for you.
For more information, email us at info@emmagoldman.com or call one of the numbers above.
Coming to the Clinic
What to Bring
Bring a valid photo ID that includes your birthdate. If using your insurance for all or part of the payment, please bring your insurance card..
If you're using a credit card for payment, make sure the cardholder is with you.
Guaranteed payment is due at the time of service. The following options for payment are acceptable:
- Cash, traveler's checks, money order, Discover/MasterCard/Visa/American Express.
- Personal checks are not accepted.
Our Building and Parking
We are easily accessible from I-380 and I-80.
Free parking is available in the south, or larger lot at the clinic. If all available spaces are taken, there is metered parking on the streets surrounding the clinic.
Protesters
Be prepared to see protesters outside our building. We encourage you to ignore them and not engage.There may be pro-choice volunteer escorts available to walk you to the front door.
Guests
Due to space and security concerns, we are currently not allowing guests to accompany clients into the building.
Late for Your Appointment
If you are late for your appointment, we may not be able to fit you into our schedule. Please call us if you’re running late or need to reschedule. We will assess appointment availability and will let you know if you will need to reschedule.
When you Arrive
A receptionist will greet you when you enter, take your payment, copy your insurance card and identification, and give you a packet of information and forms to fill out. We may collect a blood and urine sample.
Bags, Purses, Coats and jackets, including sweatshirts, are not allowed in the clinic. Please leave them in your car or at home or leave them stored in our entryway
A client advocate will accompany you throughout your stay to give you information and other supportive help. Your advocate will consult privately with you to make sure you understand the abortion procedure, aftercare instructions, and possible complications.They will also answer any questions about birth control or other matters.
We do our best to complete your appointment as quickly and safely as we can. For abortion patients, there will be a lot of waiting. Bring a book or magazine or a quiet activity to pass the time. Coffee, tea and snacks are available.
Surgical Abortion (1st Trimester)
A vacuum aspiration abortion is a safe and simple medical procedure. Vacuum aspiration is the term for the surgery used to perform a first trimester abortion. This procedure is done while you are situated in a gynecological examination position-lying down with knees bent and apart.
A speculum will be inserted into the vagina to hold the vaginal walls apart so that the cervix can be viewed easily. A local anesthetic will help numb the cervix.
The physician will attach an instrument (tenaculum) to the cervix to hold it steady before beginning the dilation. This is done by inserting successively larger dilators (long slender metal rods) through the cervix one at a time until the opening leading into the uterus is large enough to accommodate the cannula, the straw-sized tube that is used for the abortion. Most women feel cramping during the dilation.
After the cannula is inserted, the pregnancy is removed with gentle suction.A cramping sensation may be felt for two to three minutes until the abortion is over.
If you have had a surgical abortion and would like to help us by taking a survey we would appreciate it.
*Please note that in the state of Iowa, we are unable to offer abortions if cardiac activity is present at the time of the ultrasound (first visit).This generally occurs around 6-7 weeks since the first day of the last menstrual period. (LMP) Please call us if you have questions about how this might affect you.
Dilation and Evacuation (2nd Trimester)
Dilation and Evacuation or D&E is the term for the surgery used to perform a second trimester abortion. The surgery is completed in two steps:
Step one: The procedure begins with the dilation (gentle opening) of the cervix. Depending on the method used and the length of the pregnancy, dilation may be completed in a few minutes, or it may take several hours. Instruments used to dilate the cervix may include the use of dilators (long metal rods), laminaria (medicinally prepared seaweed) that absorb moisture from the body and gradually open the cervix, or a suppository/tablet called misoprostol, a prostaglandin that helps to cramp the uterus and soften the cervix.
Step two: The second part of the procedure involves the evacuation of the pregnancy and pregnancy tissue. A local anesthetic is used to numb the cervix. The uterus is emptied by using a combination of aspiration and evacuation with forceps. Most women feel menstrual like cramping during step two. Some women also experience a tugging sensation in the lower abdomen. While the uterus is returning to its non-pregnant state a woman may continue to experience cramping.
*Please note that in the state of Iowa, we are unable to offer abortions if cardiac activity is present at the time of the ultrasound (first visit).This generally occurs around 6-7 weeks since the first day of the last menstrual period. (LMP) If your pregnancy is greater than 12 weeks, please call us for information about facilities that can help you. Please call us if you have questions about how this might affect you.
Non-Surgical Abortion
The Non-surgical abortion involves the administration of two medications,Mifeprex® and misoprostol taken over 48 hours.This is NOT the same as Emergency Contraception, also known as the "Morning After Pill". To learn more about Emergency Contraception please click here..
Initially, you will be examined to determine how many weeks pregnant you are. If on ultrasound, there is no cardiac activity you will take the first medication; Mifeprex®. Mifeprex® is a medication that blocks progesterone, a hormone necessary to maintain a pregnancy. Less than 3% of women will abort the pregnancy after taking the Mifeprex®.
You will take a second medication called misoprostol up to 48 hours after the first medication. Misoprostol causes cramping and bleeding similar to or heavier than a period. This is what expels the pregnancy.
You will be scheduled for an aftercare visit or a phone call in approximately 3-4 weeks to confirm that termination of your pregnancy was complete and there have been no complications. If you would like to read more about this option, you can visit the Mifeprex® website at www.earlyoptionpill.com.
If you have had a Non-Surgical Abortion and would like to help us by taking a survery we would appreciate it.
Abortion Risks
Abortion is a safe and common medical procedure. There are various risks associated with any minor surgical procedure, including abortion. Minor complications resulting specifically from an abortion can usually be remedied by early diagnosis and treatment of the problem. Such complications occur less than one percent of the time and most commonly include, but are not limited to, perforation of the uterus, infection, excessive bleeding, incomplete or failed abortion, allergic reactions to medications, or hysterectomy. The risk of permanent damage to the reproductive organs or death resulting from an abortion is about one incidence in 150,000. (The risk of death from childbirth is 13 in 100,000)
With a non-surgical abortion, approximately 1 out of 100 women will experience bleeding so heavy that it requires a surgical procedure. Studies show a non-surgical/medical abortion is effective for 92%-95% of women who use it.
Abortion is also safe in the long-term. An uncomplicated abortion will not affect your ability to have children in the future. There is no link between abortion and breast cancer or any other ongoing physical or mental condition.
You will have an opportunity to discuss the procedure and its risks with your advocate prior to your abortion.
Post Abortion Care
Normal Recovery
Following your abortion you may experience one or more of the following:
- Spotting or bleeding which may be continuous or may start and stop several times over the three weeks following the abortion.
- No bleeding at all.
- Passing black, brown, or red blood clots.
- Cramping (abdominal or back pain)***
- Slightly elevated temperature (100 degrees or less) for a few days after you abortion.
- Emotional changes (unusually happy or depressed) for no apparent reason.
- Discharge from the nipples
- Disappearance of most pregnancy symptoms within 1 to 7 days
- Ovulation may occur at any time. Your period will come in 4 to 8 weeks.
***Cramps may be due to contraction of the uterus or to passing blood clots. Deep massage of the abdomen, downward toward the pubic bone, may help pass clots and relieve cramping. A hot water bottle or heating pad usually helps also.
Not Normal Recovery
The following is a list of symptoms that you would not experience in a normal recovery. Please be familiar with this list, and refer to it as needed during your recovery time of two weeks or until your bleeding stops:
- Bleeding or spotting for more than three weeks after your abortion.
- Heavy bleeding-soaking through 3 or more thick pads in 3 hours or less.
- Passing white, gray, or green tissue.
- Persistence of pregnancy symptoms pas two weeks following your abortion.
- Cramping so severe that you cannot stand up or continue with normal activities, or if your abdomen is tender when touched.
- Temperature of 100.4 degrees or more, steady or rising.
- Unusual, foul smelling discharge from your vagina.
- No period for more than three months.
- Severe psychological distress.
If you have any of the NOT NORMAL symptoms, call the Emma Goldman Clinic at (319) 337-2112 so we can help you decide what to do. If you cannot reach us by phone, call a doctor immediately or go to a hospital emergency room. It is important that you tell the doctor you had an abortion because that information is needed in making a correct diagnosis.
Take care of yourself by following these instructions for at least 2 weeks. If bleeding continue past 2 weeks, follow instructions until bleeding stops.
Do:
- Resume normal non-strenuous activities as soon as you wish.
- Eat healthy and iron-rich foods. Increase your fluid intake during the times you are bleeding.
- Get plenty of rest.
- Take your temperature if you feel chilled or hot.
- To minimize the chance of uterine infection:
- Use a sanitary napkin rather than a tampon
- Avoid sexual activity involving vaginal penetration
- Avoid swimming because swimming may introduce bacteria into the vagina
- Avoid douches or vaginal sprays
- Take the antibiotics that were give to you in the recovery room. You should take 1 tablet every 12 hours.
Avoid:
- Strenuous exercise for 2 to 5 days
- Alcohol and drugs which may decrease you awareness of complication symptoms.
Note:
You may use non-aspirin pain relievers (such as Tylenol, Advil, Nuprin, Midol II, Aleve) to minimize cramping. If you take pain relievers, do allow time between doses to assess the severity of pain and your temperature.
An aftercare check up in 3 weeks is important. Some complications can only be found at the aftercare examination. It is also an ideal time to arrange with your clinic doctor for whatever contraception you desire.
Have a low sensitivity urine pregnancy test three weeks after the abortion to rule out an ongoing pregnancy. This is especially important if the abortion was performed in the first 8 weeks of pregnancy.
If you were given medication in addition to the routine antibiotics, take as directed on the package.
Post Abortion Care Survey:
One Woman's Story
The Emma Goldman Clinic is inviting you, as a donor or as a client (or both!), to share your story. By sharing your experience or your reason for supporting the Clinic, you can help others understand just how essential Emma’s care is to our community. Thank you for taking the time to inspire others and help keep affordable, compassionate and inclusive reproductive health care available to people across the Midwest right here in Iowa City!
Her Story
The following unsolicited letter was received at the clinic. Minor revisions have been made to guard confidentiality.
Attending the 25th Anniversary of the Emma Goldman Clinic was a joyous experience for me. I looked around the crowd gathered on the Pentacrest, and I saw a lot of familiar faces, many now framed in gray. As the various speakers talked of serious matters in upbeat and positive language, the crowd was energized. The applause came more often, more heartily. I was proud to be at the rally, proud to be a member of the community that has, for the most part, supported and defended the clinic.
I was a teenager when the Emma Goldman Clinic was first proposed and came into fruition. It was a time of "free love." Though herpes and syphilis were possibilities, the biggest fear was pregnancy. Many of my friends saw the new clinic as a means of getting birth control. We found ourselves embarrassed to discuss it with our mothers, and shy and intimidated in the office setting of our mothers' ob-gyns. There were no female gynecologists in private practice at that time, no women's health clinics where young women could feel comfortable.
The idea of an "abortion clinic" in our community was not the way we saw the EGC. It was a women's health clinic that would offer abortions as one of many services. It wasn't a service any of us perceived needing, but one that many of us felt should be available. Of course some of us did end up needing this service. For many it seemed only a matter of time, for others an unwanted pregnancy came as a surprise.
I was twenty years old. I missed a period but thought nothing of it, after all, we'd been using birth control. But no form of birth control (except abstinence and sterilization) is foolproof. We fell in that small percentage of "failed efficiency."
I never considered having the baby. I was young, single and not financially secure. We'd been dating for several months, but what did that mean in those days? Our relationship was based more on sex than friendship, let alone love. I didn't even mention the situation to my boyfriend, or anyone else. I felt it was my decision to make, and I'd made it. I didn't know what my future would be, but I did have a pretty good idea of what lay ahead if I continued on with the pregnancy.
The women at the EGC gave me support, information, and a gentle environment. Walking home after the procedure, I felt I had made the first adult decision of my life, a responsible decision. After years of sexual encounters, I didn't reach this level of maturity until I had to face the consequences of those encounters.
The regrets I have in my life don't include abortion. I still believe it was the right decision. I know it was a decision to make. I'm certain that if it hadn't been for the Emma Goldman Clinic being available to me, I would have felt trapped and desperate. The result would have been a far different out come.
"No woman should ever have to apologize for having an abortion," and no clinic should ever have to apologize for providing a variety of safe services to women.
I thank all the people who dreamed of the Emma Goldman Clinic, and then made it a reality. I thank all the volunteers and staff who have kept the clinic going the past twenty-five years. I congratulate all those at the rally who realize the importance of continuing to support, educate and provide the community with the services given by the EGC.
------------------------------------
The Weight We Carry
After 28 years of silence, I’m finally ready to speak.
Not because my story has changed—but because the stakes have.
In today’s political climate—where reproductive freedom is under relentless attack, where young people are losing the right to plan their futures, and where shame is still being used as a weapon—I feel called to share my story.
Because the weight I carried alone back then should be shared in compassion and kindness for today’s young adults and generations to come... Read More
Personal Decision and Public Action
Today you may be discovering just how personal is the decision of whether or not to have an abortion. And, while you may need to sort through a variety of feelings about your options, we do ask you to remember that the controversies surrounding the abortion issue are far-reaching and extend to many other women besides yourself. Perhaps you already know of other friends or relatives who have faced an abortion decision. At some point in the future, abortion may touch the lives of others you know, such as friends, sisters, or daughters. It is important for those whose lives have been personally touched by this issue to aid in the defense of personal liberty and choice against the well-financed lobbies and self-righteous attitudes of those advocating the return of illegal abortion.
Today you may be discovering just how personal is the decision of whether or not to have an abortion. And, while you may need to sort through a variety of feelings about your options, we do ask you to remember that the controversies surrounding the abortion issue are far-reaching and extend to many other women besides yourself. Perhaps you already know of other friends or relatives who have faced an abortion decision. At some point in the future, abortion may touch the lives of others you know, such as friends, sisters, or daughters. It is important for those whose lives have been personally touched by this issue to aid in the defense of personal liberty and choice against the well-financed lobbies and self-righteous attitudes of those advocating the return of illegal abortion.
To help defend this personal liberty, we suggest that you
- Write your elected officials and let them know you support CHOICE.
- Identify and support pro-CHOICE candidates during political campaigning, donating your time and financial support.
- Join pro-CHOICE organizations, volunteer your time, and contribute funds to help their organized efforts to support CHOICE.
- Financially support established loan funds to help women to pay their abortion expenses.
- Express your support of CHOICE in conversations with others who will be influenced by your thoughts.
Call your city hall to find out who your elected officials are. You can write your State Representatives in care of your state capitol. You can write to your U.S. Senators and congressperson at the following addresses:
Ashley Hinson
House of Representatives
Washington, DC 20515
Senator Chuck Grassley
United States Senate
Washington, DC 20510
Senator Joni Ernst
United States Senate
Washington, DC 20510
Here are addresses of national pro-choice organizations you can join or to which you can send donations:
Abortion Care Network
1300 I Street NW, Suite 400E
Washington, DC 20005
American Civil Liberties Union (ACLU)
125 Broad St. 18th Floor
New York, NY 10004-2400
www.aclu.org
Catholics for a Free Choice
1436 U Street NW, Suite 310
Washington, DC 20009
www.cath4choice.org
Medical Students for Choice
2482 Shattuch Ave. Suite 250
Berkley, CA 94704
www.ms4c.org
National Abortion Federation
1755 Massachusetts Ave, NW Suite 600
Washington, DC 20036
www.prochoice.org
National Abortion and Reproductive Rights Action League
1156 15th St. NW, Suite 700
Washington, DC 20005
www.naral.org
National Organization for Women
1000 16th St. NW, Suite 700
Washington, DC 20036
www.now.org
Planned Parenthood of America
810 Seventh Ave
New York, NY 10019
www.plannedparenthood.org
National Network of Abortion Funds
Hampshire College
Amherst, Massachusetts 01002
www.nnaf.org
Birth Control
Abstinence
The only way to be 100% certain of preventing pregnancy is to avoid genital-to-genital contact, which means no exchange of semen or vaginal fluids. It’s important to know that pregnancy can sometimes occur without what people usually think of as “full” sexual intercourse.
Abstinence doesn’t mean the absence of closeness or intimacy. There are many ways to show love, care, and connection that don’t involve sex—like spending meaningful time together, sharing feelings, or touching in ways that feel safe and mutually comfortable.
Masturbation—touching your own genitals, or having a partner touch them with consent—is a normal and healthy way to explore pleasure. It may lead to orgasm (also called ejaculation or climax). Masturbation is safe for people of all genders and can be a positive part of caring for your body and sexuality.
At the Emma Goldman Clinic, we honor each person’s choices and experiences. Whether you choose abstinence for now, for the long term, or not at all, we’re here to provide accurate information and support in a welcoming, non-judgmental space.
Barrier Methods: Diaphragm and Other Options
How do they work?
Barrier methods prevent pregnancy by blocking sperm from reaching an egg. The diaphragm is one option: it’s a small, flexible silicone cup that fits inside the vagina and covers the cervix. For increased effectiveness, spermicide is placed in the diaphragm before insertion.
The diaphragm must stay in place for at least 6 hours after ejaculation to give the spermicide time to work, but it should not be left in longer than 24 hours. Because diaphragms come in different sizes, a health care provider needs to fit you for one.
How effective is it?
With typical use, the diaphragm is about 82–94% effective. Effectiveness improves when it’s used consistently and correctly, every time.
What’s good about the diaphragm?
- Provides some protection against sexually transmitted infections (STIs).
- Non-hormonal, so there are fewer side effects compared to birth control pills, implants, or IUDs.
- Can be used only when needed, not every day.
What are the drawbacks?
- Insertion and removal can feel tricky at first.
- Must be used every time you have sex.
- Can slightly increase the risk of urinary tract infections (especially if the diaphragm is too large or not fitted properly).
Other Over-the-Counter Barrier Options
- External condoms (worn on the penis) – Available in many sizes and materials, they protect against both pregnancy and STIs. Easy to buy over the counter.
- Internal condoms (worn inside the vagina or anus) – Offer pregnancy and STI protection, and can be inserted ahead of time. Available without a prescription.
- Contraceptive sponge – Contains spermicide and fits over the cervix. It can be purchased without a prescription, used for up to 24 hours, and does not require a fitting.
- Cervical cap – Smaller than a diaphragm, it also covers the cervix and is used with spermicide. Some types are available by prescription, though others may be accessible online.
At the Emma Goldman Clinic, we believe everyone deserves options. Whether you’re interested in prescription methods like the diaphragm, or over-the-counter barriers you can buy at a pharmacy, our staff can help you find what works best for your body, your needs, and your life.
Hormonal Birth Control
At Emma Goldman Clinic, we know that people of many genders may use birth control. The information below is written with inclusive language so that everyone can feel respected in their reproductive health decisions.
Birth Control Pills (The Pill)
How they work
Birth control pills contain hormones (estrogen and/or progesterone) similar to the ones made naturally by the body. Pills usually prevent the release of an egg (ovulation). They also thicken cervical mucus, making it harder for sperm to reach an egg.
- Pills are taken daily for 3 weeks, followed by 1 week of non-hormone “placebo” pills. During this week, bleeding similar to a period usually occurs (often lighter and shorter).
- Pills must be taken at the same time every day to work best.
Effectiveness
- About 97–99.9% effective with correct, consistent use.
- Effectiveness can be reduced by:
- Taking pills late or skipping doses
- Certain medications (such as antibiotics or seizure drugs)
- Vomiting or diarrhea soon after taking a pill
- Taking pills late or skipping doses
What’s good about the pill
- Periods are often lighter and less crampy
- Doesn’t interrupt sex
- May improve acne and PMS symptoms
What’s not so good
- Daily commitment can be difficult for many people
- No protection against sexually transmitted infections (STIs)—condoms are still needed
- Possible side effects: nausea, weight gain, vaginal infections, acne
- Not recommended for some people with health conditions or who smoke (increased risk of blood clots, stroke, heart attack)
Depo-Provera (The Shot)
How it works
Depo-Provera is an injection of a hormone called medroxyprogesterone acetate, given every 12 weeks. It prevents ovulation, thickens cervical mucus, and thins the uterine lining.
Effectiveness
- About 99.7% effective when injections are given on schedule.
What’s good about the shot
- Only needed every 3 months
- Estrogen-free, so it can be used by people who can’t take estrogen
- Private and convenient
- Many people have fewer cramps or stop bleeding after a year of use
What’s not so good
- Irregular bleeding is common at first
- Side effects may include weight gain, headaches, acne, mood changes, lower sex drive
- Fertility may take 6–24 months to return after stopping
- Possible temporary bone loss (improves after stopping)
- No STI protection
⚠️ When to seek care right away (ACHES):
- A: Severe abdominal pain
- C: Chest pain or trouble breathing
- H: Severe headaches, dizziness, or fainting
- E: Eye problems such as blurred vision
The Patch (Ortho Evra / Xulane)
What it is
A small adhesive patch worn on the skin that slowly releases estrogen and progestin. Prevents ovulation, thickens cervical mucus, and thins uterine lining.
How to use
- Place on clean, dry skin (not on the chest).
- Wear for 1 week at a time. Replace weekly for 3 weeks, then go without a patch for 1 week (bleeding usually occurs).
- Always check that the patch is sticking properly.
Effectiveness
- About 99% effective with correct use
- Slightly less effective for people weighing more than 198 lbs
What’s good about the patch
- Weekly schedule (instead of daily pills)
- Doesn’t interrupt sex
- Predictable bleeding
What’s not so good
- Can cause skin irritation at the site
- No STI protection
- Not recommended for people 35+ who smoke (higher risk of clots, heart attack, stroke)
- May interact with some medications (like certain antibiotics, seizure meds, or herbal remedies)
The Ring (NuvaRing)
What it is
A small, flexible vaginal ring that releases estrogen and progestin. Worn inside the vagina for 3 weeks, then removed for 1 week (bleeding occurs).
How to use
- Insert within 5 days of starting a period for immediate protection
- Leave in place for 3 weeks, remove for 1 week, then insert a new ring
- Only 1 ring should be used at a time
Effectiveness
- Highly effective when used correctly
What’s good about the ring
- Monthly routine instead of daily or weekly
- Discreet—may not be noticeable to a partner
- Doesn’t interrupt sex
- Predictable bleeding
What’s not so good
- No STI protection
- May cause vaginal irritation or increased discharge
- Some people experience spotting, headaches, breast tenderness, or mood changes
- Not recommended for people 35+ who smoke (same clot risks as other estrogen methods)
✨ Key Takeaway
Hormonal birth control (pills, shot, patch, ring) are all safe and effective ways to prevent pregnancy. Each has unique pros and cons, so the right choice depends on your health, lifestyle, and comfort.
👉 Remember: None of these methods protect against STIs. Using condoms is the best way to reduce your risk of infections.
LARC (IUD, Implants)
What is an implant?
The contraceptive implant is a small, flexible rod (about the size of a matchstick) that is placed just under the skin of your upper arm by a health care provider. It slowly releases a progestin hormone (etonogestrel) that prevents pregnancy. The most common brand in the U.S. is Nexplanon®.
How does it work?
- Thickens cervical mucus, which helps block sperm from reaching an egg.
- Prevents ovulation (the release of an egg from the ovary).
- Thins the lining of the uterus, making it less likely for a fertilized egg to implant.
How effective is it?
The implant is more than 99% effective at preventing pregnancy. Because it doesn’t depend on daily or monthly use, it’s one of the most reliable methods available.
How long does it last?
The implant provides protection for up to 3 years but can be removed at any time if you decide you want to become pregnant or switch to another method. Fertility usually returns quickly after removal.
Benefits of the implant
- Highly effective and reversible.
- Private—nothing to remember before or after sex.
- Can reduce menstrual cramps, and some people have lighter or no periods while using it.
- Safe for most people who cannot or prefer not to use estrogen-containing birth control.
Possible side effects
- Irregular bleeding patterns (may be lighter, heavier, or unpredictable).
- Headaches, acne, or mood changes.
- Arm soreness or bruising at the insertion site (usually temporary).
Things to consider
- Does not protect against sexually transmitted infections (STIs)—using condoms is recommended for STI prevention.
- Requires insertion and removal by a trained health care provider.
What is an IUD?
The intrauterine device (IUD) is a plastic device that is put into the uterus to prevent pregnancy. There are two kinds used in the United States. One contains copper wire and the other an artificial women's hormone (a progestin) called levonorgestrel. The copper IUD may remain in the uterus for 10 years. The progestin IUD must be replaced after 5 years when much of the hormone has been used. Both of the IUDs are "T" shaped.
How Does it Work?
There are several theories on how IUDs work, but no one knows for sure. The IUD may prevent fertilization (the joining of the egg and sperm) or it may prevent the fertilized egg from implanting and growing on the wall of the uterus. Here are some of the theories:
- There may be increased movement (muscle contractions) in the uterus and uterine tubes and that may prevent fertilization or implantation
- There may be an inflammatory response which prevents fertilization or implantation.
- There may be increased numbers of white blood cells from the imflammation (and also from progestin in the progestin IUD) which destroy sperm and the fertilized egg.
- Progestin prevents the growth of the lining of the uterus. It also causes cervical mucus to be thicker which decreases sperm movement. It also contains many white blood cells that destroy sperm.
- Copper may decrease sperm movement, ability to combine with the egg, and it also destroys sperm.
- There may be increased production of prostaglandins that may interfere with implantation.
How effective are IUDs?
Effectiveness depends on whether the woman checks for placement of the IUD string at the cervical opening. Women who check the string every time before intercourse will have higher effectiveness rates. Both theoretical and use effectiveness rates of the two newer IUDs are greater than 99%.
IUDs are more likely to be expelled from the uterus in the first 3 months after insertion.
How is the IUD put into the uterus?
IUDs should be inserted during a menstrual period. It is more comfortable because the cervix (the neck of the uterus which is in the vagina) is softer and the cervical os (its mouth or opening) is more open at that time. Also, women are much less likely to be pregnant if they are having a period.
Most women feel some cramping during insertion of the IUD and for several minutes after insertion. Some report cramping for a day or two after and sometimes during the first few menstrual periods.
Complications of IUD use
Pelvic Inflammatory Disease (PID)
PID is an infection of the uterus and sometimes of the tubes, ovaries, and even the abdominal cavity. The risk of PID is much lower if you and your partners have no other partners. If you suspect that you may have a sexually transmitted infection (STI), like gonorrhea or chlamydia, see a health care provider immediately for treatment. It is important to be tested for STIs at least once a year or whenever you suspect that you may have been exposed. Symptoms of PID are a foul smelling discharge, pelvic pain or tenderness, severe cramping, or a fever.
PID can cause scarring of the uterine tubes which can lead to the inability to have children or an increased chance of having a pregnancy in the tube. The tube ruptures around 8 to 12 weeks of a pregnancy. This may result in severe bleeding which can cause death.
PID can cause chronic pelvic pain from scarring in the abdominal cavity. The infection alone can also result in death if the woman is not put on antibiotics soon enough.
Embedding or perforation
The IUD can work its way partly through, or all the way through the uterine wall. There may or may not be pain as this is happening. Guard against this by checking for the string before intercourse, or at least once a month.
The health care practitioner may injure the uterine wall during insertion. The injury may go all the way into the abdominal cavity. This is also called perforation. The perforation will heal, usually needing no treatment.
Expelling the IUD
A woman's uterus sometimes contracts and pushes the IUD out. This is more likely to happen in the first 3 months of use. There may be vaginal discharge and pain or lengthening of the string. Or there may be no indications that this is happening. It is very important to check for the string regularly.
Pregnancy with an IUD in place
If a pregnancy does occur, there is a 50% chance that the woman will have a miscarriage. She is at higher risk for infection with the IUD in place. If the IUD is removed, there is a 25% chance of a miscarriage.
Getting pregnant after removal of an IUD
It is best to wait at least 3 months after having an IUD removed to try to get pregnant. The uterine lining needs time to return to normal functioning and it may decrease the risk of an ectopic pregnancy.
Benefits of the progestin IUD - Mirena
This IUD releases 20 micrograms of progestin a day. Studies have shown:
- Lighter periods with less cramping and bleeding - up to 88% less blood loss
- Decreased bleeding at menopause - may avoid hysterectomy
- Decreased growth of uterine lining with estrogen replacement therapy
- Decreased pelvic infections, therefore, fewer ectopic pregnancies
Side effects of the progestin IUD - Mirena
- no periods
- acne
- headaches
- nausea
- breast tenderness
Contraindications to getting an IUD
You should not have an IUD if you:
- Are pregnant
- Have PID or a history of PID
- Have endometriosis
- Have been exposed to or have gonorrhea or chlamydia
- Have confirmed or suspected cancer of the cervix or uterus
- Undiagnosed abnormal vaginal bleeding
- Blood clot or bleeding disorder
- Acute liver disease
- Have abnormalities of the uterus such as those present from birth or possibly fibroids
- Consider another birth control method if:
- You have more than one partner or a partner with more than one partner
- You are unable to check the IUD string, especially if your partner is also unable to check the string
✨ At the Emma Goldman Clinic, we provide supportive, non-judgmental care to help you decide if the implant—or any other LARC method—is right for you. Your body, your choice, your timeline.
Fertility Awareness
How does it work?
Fertility awareness, sometimes called “natural family planning,” involves tracking your body’s natural signs of fertility to know which days you are most likely to get pregnant. By avoiding sex or using another form of protection on those days, you can reduce the chance of pregnancy.
Ways to track fertility:
- Cervical secretions:
During your cycle, cervical mucus changes in texture and appearance. Fertile mucus is usually clear, stretchy, and slippery—similar to raw egg whites. This fertile mucus helps sperm live inside the body for 5–10 days. Ovulation usually happens within 24 hours of the last day of fertile mucus. - Basal body temperature (BBT):
Your resting temperature rises slightly (about 0.6°F or more) after ovulation. By taking your temperature at the same time every morning before getting out of bed and charting the results, you can confirm when ovulation has already happened. Keep in mind that BBT shows fertility after the fact—meaning you may already be at risk if you had unprotected sex in the days before. - Calendar (rhythm method):
This method assumes ovulation happens at mid-cycle. Because many people do not ovulate on the same day each month, calendar-only tracking is much less reliable than checking mucus or BBT.
How effective is it?
Effectiveness varies widely depending on how consistently and correctly the methods are used. Studies show success rates from 80% to 98%. Fertility awareness is more effective when practiced with careful daily tracking and partner cooperation.
What’s good about it?
- Non-hormonal, with no medical side effects.
- Encourages body awareness and self-knowledge.
- Can be used to prevent pregnancy or to help plan pregnancy.
What’s not so good?
- Requires daily attention, careful tracking, and time to learn.
- May involve many days of abstinence or condom use each month.
- Less effective if cycles are irregular or if instructions are not followed carefully.
- Does not protect against sexually transmitted infections (STIs).
Where can I learn more?
The Emma Goldman Clinic publishes Fertility Awareness: A Natural Way to Avoid or Achieve Pregnancy, a resource that teaches how to recognize fertility signs and track your cycle. This guide helps you take an active role in your reproductive health and can be paired with other self-care practices, like breast and cervical self-exams.
📖 You can purchase the book for $7 at the Emma Store and download a mucus and temperature chart to track your reproductive cycle.
✨ At the Emma Goldman Clinic, we support informed choices. Fertility awareness can be empowering, but it works best when you have the time, motivation, and support to track your body’s signals carefully.
Natural Birth Control
How does it work?
CHECKING CERVICAL SECRETIONS
There are many types of natural birth control methods. The most effective natural method is checking cervical secretions for the wet and slippery, clear and stretchy fertile mucus. Sperm can live in the fertile mucus for 5 to 10 days or more. You ovulate within 24 hours of the last day of clear stretchy mucus.
BASAL BODY TEMPERATURE
Basal body temperature indicates when ovulation (release of an egg from the ovary) has occurred, but that is too late if you had sex the night before when fertile mucus is present. You check and chart the temperature daily for 6 months. Look for a drop in the temperature and then a rise of al least 0.6 of a degree that stays up for at least 3 days.
RHYTHM
Rhythm (periodic abstinence) is going by the calendar and assuming you ovulate at mid-cycle. Many women do not always ovulate at mid-cycle, and so just using the calendar method is very unreliable.
How effective is it?
Effectiveness varies a great deal depending on the method and the users. It ranges from 80% to 98% in different studies.
What's good about it?
It does not harm your body in any way. You learn about how your body works.
What's not good about it?
It is not very effective for many people. It takes a while to learn the method(s) and become skilled in using them. It requires very high motivation on the part of the user, and it requires full cooperation from the woman's partner. It may require many days of abstinence each month. It does not protect against sexually transmitted infections.
Where can I learn more about this method?
The Emma Goldman Clinic publishes a book titled Fertility Awareness: A Natural Way to Avoid or Achieve Pregnancy. This book is about a natural way to control fertility by learning to identify the physical changes that accompany the different phases of the menstrual cycle. By learning to recognize these changes as they occur, you can plan which days are safe or unsafe to have sexual intercourse if you are trying to prevent conception, or which days are best for conception if you are planning a pregnancy. In addition to controlling fertility, the techniques for recognizing cycles of fertility can help you become an intelligent participant in your own health care, when used in conjunction with other self-health skills such as breast and cervical self-exams.
Click here to visit the Emma Store where you can purchase Fertility Awareness: A natural way to avoid or achieve pregnancy for only $7.
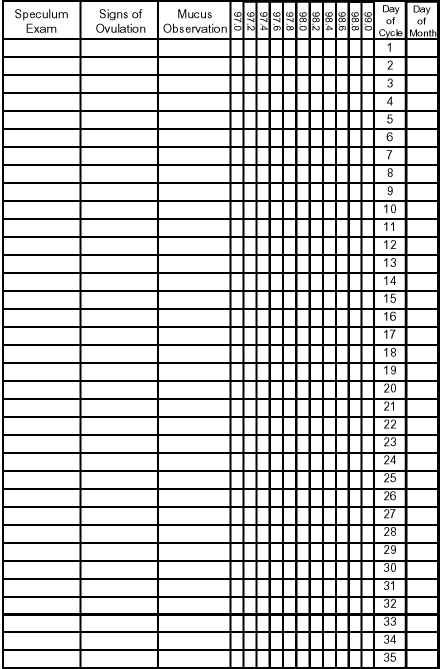
The chart below is to help you keep track of your reproductive cycle, as instructed in our book. You can fill in what mucus you observed, and what your basal body temperature was for each day. You can click this link to open the chart as a pdf that you can save on your computer. You can also use the chart displayed below.
Emma Goldman Clinic
227 N. Dubuque Street
Iowa City, IA, 52245
319-337-2111
800-848-7684
info@emmagoldman.com
Spermacides
What are they?
Spermicides are products that kill sperm and help prevent pregnancy. They come in several forms, including gel, foam, cream, film, suppositories, and sponges. All types are placed inside the vagina before sex.
Some spermicides need to be in place at least 10–15 minutes before sex to work effectively. If more than an hour passes before sex, or if you have sex again, you need to apply more spermicide.
How effective are they?
When used alone, spermicides are about 79–94% effective at preventing pregnancy. Effectiveness improves when they are used together with another barrier method, such as condoms.
What’s good about spermicides?
- Available over the counter—no prescription needed.
- Easy to use and convenient for people who prefer a non-hormonal method.
- More effective when combined with condoms, which also protect against sexually transmitted infections (STIs).
What’s not so good?
- Can cause genital irritation or burning for some people.
- Some find them messy or feel they interrupt intimacy.
- Must be reapplied before each act of intercourse.
Foam and suppositories
- Foam: a fluffy, white cream that is inserted into the vagina with an applicator. Foam should be used within 15 minutes before sex and must be reapplied before each act of intercourse.
- Suppositories: small, solid tablets inserted into the vagina, where they dissolve near the cervix. They should be placed at least 10 minutes before sex and protect for about 2 hours. A new suppository is needed for each act of intercourse.
Effectiveness with other methods
Using spermicide with a condom makes pregnancy prevention much more effective—lowering the chance of pregnancy to 2–7% per year. This combination also provides protection against STIs.
✨ At the Emma Goldman Clinic, we encourage combining spermicides with barrier methods like condoms for safer and more effective protection. Our staff can help you explore whether spermicide fits your needs and how to use it in combination with other methods that affirm your body, your choices, and your health.
Tubal Ligation
Tubal ligation—sometimes called “female sterilization” or “band-aid surgery”—is currently the most effective form of birth control available, other than abstinence. Many people choose this method when they are certain they do not want any or any more children. For those who choose it, it can bring freedom from the fear of pregnancy and allow for increased sexual enjoyment and spontaneity.
Important Considerations
- Permanent procedure: Tubal ligation should be considered irreversible. While reversal surgeries exist, they are costly, risky, and rarely successful.
- Surgical risks: It is a major surgical procedure with higher risks and costs than male sterilization (vasectomy).
- Costs: Typical costs range from $800–$3,000 (a one-time expense).
- Counseling advised: We strongly recommend discussing both female and male sterilization options before making a final decision.
How It Works
Tubal ligation blocks or interrupts the fallopian tubes, preventing the egg and sperm from meeting.
- You will still ovulate (release eggs) and menstruate.
- Hormone levels remain within normal limits, though serum progesterone may be slightly reduced.
Surgical Options
Abdominal Procedures
- Laparoscopy (“band-aid surgery”):
A small incision near the navel allows insertion of a lighted instrument. Gas is used to lift the abdominal wall, giving the surgeon a clear view. Tubes are then closed using cauterization, bands, rings, clips, or by cutting and tying. - Minilaparotomy:
The uterus is gently lifted toward the abdominal wall, and a small incision is made above it. The tubes are then cut, tied, burned, or clipped.
Vaginal Procedure
- Colpotomy:
An incision is made in the vagina behind the cervix, and the tubes are tied or clipped. This is easier for those who have had children, but it carries a higher risk of complications and pregnancy than abdominal procedures.
Methods of Closing the Tubes
- Cutting and tying – safest and most effective, with the longest track record.
- Cauterization (burning) – higher risk of accidental injury to other organs.
- Rings, bands, or clips – newer, still being studied.
- Silicone plugs – experimental, with limited research.
Possible Complications
- Menstrual changes: heavier bleeding, more cramping, or irregular cycles.
- Ectopic pregnancy risk (pregnancy outside the uterus, often in the tube).
- Failure of closure: tubes may heal and reconnect.
- Rare: early menopause or injury to other organs.
- Regret over permanent loss of fertility.
Reversibility
While some women have undergone reversal surgery, success rates are low. Tubal ligation should never be chosen with the expectation of reversal. Medicaid and most insurance programs cover sterilization but not reversals.
Sterilization Abuse & Consent
Historically, some women—especially low-income and minority women—were sterilized without full consent. True informed consent means:
- No pressure to sign during labor or while under anesthesia.
- Consent forms must be in a language the patient understands.
- The choice must be completely voluntary.
Any woman seeking sterilization has the right to the procedure regardless of age, marital status, or number of children. Spousal consent is not required.
✅ For more information or referrals, contact your local family planning clinic.
❌ A hysterectomy (removal of the uterus) should never be performed solely for sterilization.
Withdrawal
How does it work?
Withdrawal means the penis is removed from the vagina before ejaculation, so semen does not enter the vagina.
How effective is it?
Withdrawal is about 81–96% effective, depending on how consistently and correctly it is used. Effectiveness depends on a person’s ability to recognize when they are about to ejaculate and withdraw in time.
It’s important to note that many people release pre-ejaculate (“pre-cum”) before ejaculation. While it usually contains fewer sperm, it can still cause pregnancy. This makes withdrawal less reliable than most other birth control methods.
What’s good about it?
- Free, widely available, and no prescription needed.
- No hormones, no medical side effects.
- Can help people and partners learn more about their bodies, arousal, and sexual response.
What’s not so good?
- Not as effective as most other methods.
- Requires practice, awareness, and trust between partners.
- Does not protect against sexually transmitted infections (STIs).
- Can cause stress or interrupt intimacy.
Best use tip: Withdrawal is more effective when combined with other methods (such as spermicides or condoms).
✨ At the Emma Goldman Clinic, we honor that people make different choices based on their needs and situations. If withdrawal is your method—or if you’d like to explore more effective options—we’re here to provide non-judgmental support and accurate information.
Vasectomy
A vasectomy is a safe, simple, and permanent method of birth control for people with testes who are sure they do not want to cause a pregnancy in the future. It is one of the most effective options available.
During the procedure, the tubes that carry sperm from the testicles (the vas deferens) are closed or blocked. This keeps sperm from mixing with semen. After healing, ejaculation and orgasm feel the same as before—the semen just no longer contains sperm. Hormones, erections, and sex drive are not affected.
Why choose vasectomy?
- Over 99% effective at preventing pregnancy
- Quick procedure (usually 15–30 minutes)
- Lower risk, cost, and recovery time compared to tubal ligation
- One-time procedure, no ongoing supplies or prescriptions
Things to keep in mind:
- Considered permanent—reversal is difficult, costly, and not always successful
- Not immediately effective; sperm can remain in semen for a few months after surgery, so backup birth control is needed until follow-up testing confirms no sperm are present
- Does not protect against sexually transmitted infections (STIs)—condoms are still important for STI prevention
At Emma Goldman Clinic, we believe in informed choice. We can provide information and referrals for vasectomy, and we’ll support you in deciding if it’s the right option for your body, your life, and your future.
Emergency Contraception: A Second Chance at Birth Control
What is it?
Emergency contraception (EC) can reduce the chance of pregnancy after unprotected sex or when another birth control method fails. EC is most effective the sooner you take it, but depending on the type, it can work up to 5 days (120 hours) after unprotected sex.
EC is a contraceptive—it cannot end an existing pregnancy and is not the same as the abortion pill (mifepristone, sometimes called RU-486). EC also does not protect against sexually transmitted infections (STIs) and is not intended to be used as your primary or ongoing birth control method. Think of it as a “second chance” option.
Didn’t they used to call it the “Morning After Pill”?
Yes. Emergency contraception has been called the “morning after pill,” but that name can be misleading. Because EC can be taken up to 5 days after unprotected sex, the term “emergency contraception” (or by brand name, such as Plan B One-Step® or ella®) is more accurate.
When might I need EC?
People use EC in situations such as:
- A condom broke, slipped, or wasn’t used.
- A birth control pill was missed or taken late.
- A diaphragm, cap, or sponge slipped out of place.
- A Depo-Provera® shot was missed.
- You experienced pressure, coercion, or sexual assault.
- It was your first time having sex and protection wasn’t used.
How does it work?
EC pills mainly work by delaying or preventing ovulation (the release of an egg). Without an egg, sperm cannot cause pregnancy. FDA-approved EC pills do not disrupt an implanted pregnancy.
- Levonorgestrel pills (Plan B One-Step® and generics): Most effective within 72 hours but may work up to 5 days. Available over the counter without age restriction.
- Ulipristal acetate (ella®): Effective up to 5 days after sex and may be more effective than Plan B, especially for people with higher body weight. Prescription required.
- Copper IUD (ParaGard®): The most effective EC option. Must be inserted by a provider within 5 days of unprotected sex and provides long-term birth control for up to 10 years.
How effective is EC?
- Plan B One-Step® reduces the risk of pregnancy by about 75–89% when taken within 3 days.
- ella® is more effective than Plan B, particularly later in the 5-day window.
- A copper IUD is over 99% effective when used as EC.
Is EC safe?
Yes. EC has been approved by the FDA as a safe way to lower the chance of pregnancy after unprotected sex. Side effects are usually mild and short-term.
Possible side effects:
- Nausea or upset stomach
- Headache or dizziness
- Breast tenderness
- Changes in timing of your next period (it may come earlier or later than expected)
These effects usually last a day or less. EC will not affect your ability to get pregnant in the future.
Where can I get EC?
- Plan B One-Step® and generics: Available at most pharmacies, grocery stores, and clinics—no prescription or age restriction.
- ella®: Available with a prescription.
- Copper IUD: Available at clinics like the Emma Goldman Clinic.
You can purchase Plan B One-Step® directly from the Emma Goldman Clinic during our open hours: Monday–Friday, 9:00 a.m. to 5:00 p.m.
✨ At the Emma Goldman Clinic, we provide emergency contraception and compassionate care. Whether you need EC today or want to talk about ongoing birth control options, we’re here to support you in a safe, non-judgmental space.
STI's
General Information
STIs are more common and more severe now than they have been in the recent past. In addition to the more familiar bacterial infections (such as gonorrhea, syphilis and chlamydia), the contraction of viral infections has increased dramatically. The most common sexually transmitted viral infections are known as the four H-viruses. They may be transmitted through sex and last a person's entire life. The H-viruses are:
- Human Immunodeficiency Virus (HIV)
- Herpes Simplex Virus
- Hepatitis B Virus
- Human Papilloma Virus (including genital warts)
No cure exists for these infections caused by viruses. In the case of HIV, the infection can lead to death.
Preventing the spread of infection is the best way to reduce the numbers of STIs. In general, the things you can do to protect yourself from HIV will also protect you from gonorrhea, chlamydia, herpes, genital warts, and other STIs. Here are several things you can do to protect yourself from STIs:
- Abstain from all sexual activity with another person
- Be sexually intimate with only one person, who is only sexually intimate with You (this is called mutual monogamy), when both of you are known to be Uninfected, and when trusting each other to be faithful is realistic and practical
- Abstain from all sexual activities that could possibly result in the exchange of Infected body fluids (such as blood, vaginal secretions, semen, and saliva) Including vaginal, anal and oral sex, and also abstain from wet kissing when lips, Gums or other tissues are raw or bleeding
- Do not share injection equipment or needles of any kind
- Be sexually intimate only when latex condoms, dental dams, rubber gloves, Or other barriers are used to prevent exchange of semen, blood, and vaginal Secretions (a spermicidal lubricant may be beneficial at the time of sex)
You may feel embarrassed and scared if you think you have been exposed to an STI, but asking for information and getting treatment are better than worrying and getting sicker. It is also extremely important that you talk to your partner about STIs and sexual histories. Even if it is uncomfortable to do, it can save your life. In some cases, it can even improve your relationship, like in the following case.
"I fell in love with a girl and just prior to having intercourse she told me she had herpes on the outer lips of her vagina. We did not have intercourse that night. Later, as we grew closer, I came to trust her. We decided that we could cooperate in taking precautions to prevent me from getting herpes. We used condoms every time. We had a beautiful relationship. I never got infected. Her conditions actually made our relationship deeper and closer because we trusted and cooperated with each other."
If you are not comfortable enough with your partner to talk about STIs, you should not be having sex.
I Don't Know Him Well Enough to Look!
A patient in a clinic had herpes and genital warts. When asked if her partner had any warts or lesions she replied, "I don't know him well enough to look." Although she knew this man well enough to have sex with him and to get two STIs from him, she didn't feel she knew him well enough to look at his penis.
The health information provided on emmagoldman.com is not intended or implied to be a substitute for professional medical advice. Nothing stated by this website or linked pages should be used for medical diagnosis or treatment. If you have an urgent medical problem call 911 immediately or contact your healthcare provider.
Taking Steps to Protect Your Sexual Health
Ways to Take Care of Your Sexual Health
Lower-risk activities include:
- Massages
- Hugging and cuddling
- Kissing (closed-mouth)
- Solo masturbation
- Hand-to-genital touching
- Mutual masturbation
Activities with some risk (risk is lower when barriers are used):
- Open-mouth (“wet”) kissing
- Vaginal or anal sex with a condom (adding water-based or silicone lube reduces irritation; spermicide may add protection but can also cause irritation for some people)
- Oral sex on a penis with a condom
- Oral sex on a vulva/vagina with a barrier (such as a dental dam), especially important if there is bleeding or infection present
Higher-risk activities (greater chance of STI transmission):
- Any vaginal or anal sex without a condom or barrier
- Oral sex without a condom or barrier
- Oral sex on a vulva/vagina during menstruation or with infection when not using a barrier
- Oral–anal contact without protection
- Sharing sex toys without cleaning or covering them between partners
- Blood-to-blood contact of any kind (including menstrual blood, shared needles, or sexual activity that causes bleeding)
💡 Remember: Taking steps to protect your sexual health isn’t about judgment—it’s about making choices that align with your values, comfort, and care for yourself and your partners.
Chlamydia
Symptoms
Many people with chlamydia have no symptoms at all. When symptoms do appear, they can take a long time to develop and may include:
- For people with a penis: painful or burning urination, watery or milky discharge from the penis.
- For people with a vagina: abnormal discharge, irregular bleeding, pelvic pain sometimes accompanied by nausea and fever, painful or frequent urination.
Because people with a vagina are less likely to notice symptoms, it’s important to get regular STI screenings and bacterial culture tests if you are sexually active.
Treatment
Chlamydia can be treated and cured with antibiotics such as doxycycline or tetracycline. Completing the full course of medication is essential, even if symptoms go away.
If untreated
If left untreated, chlamydia can lead to serious health complications. For people with a uterus, it can cause pelvic inflammatory disease (PID), which may lead to chronic pain, ectopic pregnancy, or infertility. For all people, untreated infection can increase the risk of contracting or transmitting other STIs, including HIV.
Important Note
The health information provided on emmagoldman.com is not intended or implied to be a substitute for professional medical advice. Nothing stated on this website or linked pages should be used for medical diagnosis or treatment. If you have an urgent medical problem, call 911 immediately or contact your healthcare provider.
Gonorrhea
Symptoms
Gonorrhea doesn’t always cause noticeable symptoms—many people never know they are infected without testing. When symptoms do appear, they may look different depending on the body parts involved:
- Possible symptoms for people with a penis:
- Burning or painful urination
- Penile discharge (white, yellow, or green)
- Swelling or pain in the testicles
- Fever or painful sex
- Burning or painful urination
- Possible symptoms for people with a vagina:
- Pain in the pelvic area
- Unusual vaginal discharge
- Irregular bleeding (including after sex)
- Burning with urination
- Symptoms similar to those seen in people with a penis
- Pain in the pelvic area
- Other possible symptoms (anyone):
- Sore throat (if infection is in the pharynx)
- Rectal discomfort, discharge, or bleeding (if infection is anal)
- Sore throat (if infection is in the pharynx)
Treatment
Gonorrhea can be cured with antibiotics. Current CDC guidelines recommend dual therapy, usually with an injection of ceftriaxone and sometimes combined with oral medication. (Older treatments, such as penicillin alone, are no longer effective because the bacteria has developed resistance.)
If untreated
Without treatment, gonorrhea can cause serious complications:
- For people with a uterus, untreated infection can spread to the fallopian tubes, leading to pelvic inflammatory disease (PID), scarring, and infertility.
- For people with a penis, untreated infection can lead to painful swelling of the epididymis and, in rare cases, infertility.
- For all people, untreated gonorrhea increases the risk of contracting or transmitting HIV.
The longer gonorrhea is left untreated, the greater the risk of long-term, irreversible damage. Regular testing and early treatment are the best protection.
⚠️ Medical Disclaimer
The health information provided on emmagoldman.com is for educational purposes only and is not intended as a substitute for professional medical advice. Nothing on this website or linked pages should be used for medical diagnosis or treatment. If you have an urgent medical problem, call 911 immediately or contact your healthcare provider.
Syphillis
Symptoms by Stage
Syphilis progresses in stages. Symptoms can vary widely or sometimes not appear at all.
- Primary stage: a single, painless sore (called a chancre) at the site where the bacteria entered the body, usually appearing 3–6 weeks after exposure.
- Secondary stage: rash (often on the palms or soles), swollen lymph nodes, fever, sore throat, muscle aches, fatigue, or patchy hair loss.
- Latent stage: no visible symptoms, but the bacteria remain in the body. This stage can last for years.
- Tertiary (late) stage: if untreated, syphilis can lead to severe health problems including neurological damage, blindness, dementia, heart disease, aneurysms, and even death.
Diagnosis
Syphilis is diagnosed with a simple blood test. Sometimes a swab of a sore can also detect the bacteria. Regular testing is essential if you are sexually active, especially with new or multiple partners.
Treatment
Syphilis is curable with antibiotics, usually a shot of penicillin. For people allergic to penicillin, other antibiotics such as doxycycline may be prescribed. Treatment is most effective in the early stages but can still prevent further damage in later stages.
It is important that:
- All sexual partners are tested and treated to avoid reinfection.
- You avoid sexual contact until treatment is complete and follow-up tests confirm the infection is gone.
If Untreated
Without treatment, syphilis can progress to the tertiary stage, causing permanent damage to the brain, eyes, heart, and other organs. Serious complications include:
- Neurological problems (stroke, paralysis, dementia)
- Blindness
- Heart disease and aneurysms
- Death in severe cases
⚠️ Medical Disclaimer
The health information provided on emmagoldman.com is for educational purposes only and is not intended as a substitute for professional medical advice. Nothing on this website or linked pages should be used for medical diagnosis or treatment. If you have an urgent medical problem, call 911 immediately or contact your healthcare provider.
Herpes
Symptoms
Genital herpes may cause:
- Pain, itching, or burning in the genital area
- Blisters that break and become sores
- Burning or pain during urination
- Vaginal or penile discharge
- Pressure or tingling in the genital area
The first outbreak is usually the most uncomfortable and may last 7–10 days. Later outbreaks are typically milder and shorter (4–5 days). Over time, outbreaks often become less frequent.
Some people also experience flu-like symptoms during the first outbreak, such as fever, swollen glands, body aches, or fatigue. Others may not notice symptoms at all.
How Do I Know If I Have Herpes?
If you notice sores, blisters, or other symptoms, a healthcare provider can often diagnose herpes by examining the area. A swab test of an open sore or a blood test can confirm the infection.
How Soon Do Symptoms Appear?
Symptoms, if they occur, usually appear within 2–12 days after exposure. Some people don’t notice symptoms for weeks, months, or even years.
Treatment
While herpes cannot be cured, medications can help:
- Antiviral medications such as acyclovir (Zovirax), valacyclovir (Valtrex), or famciclovir (Famvir) can shorten outbreaks, ease symptoms, and reduce the chance of passing herpes to partners.
- Pain relievers (like ibuprofen) can help with discomfort.
- Self-care tips include keeping the area clean and dry, wearing loose cotton underwear, applying cool compresses, or using warm baths to ease pain.
Some people explore natural or complementary remedies (such as applying aloe vera or using stress reduction practices). While these may help with comfort, only antiviral medications are proven to reduce outbreaks and transmission.
Preventing the Spread of Herpes
- Use condoms or dental dams during oral, vaginal, or anal sex—especially when symptoms or sores are present.
- Avoid sexual contact during outbreaks.
- Daily antiviral medication can significantly reduce the risk of passing herpes to partners.
- Open, honest conversations with partners about STI status and testing can build trust and help protect everyone’s health.
Pregnancy and Herpes
If you are pregnant and have herpes, let your healthcare provider know. Most people with herpes have healthy pregnancies and births. If there is an active outbreak at the time of delivery, a Cesarean section (C-section) may be recommended to protect the baby from infection.
⚠️ Medical Disclaimer
The health information provided on emmagoldman.com is for educational purposes only and is not intended as a substitute for professional medical advice. Nothing on this website or linked pages should be used for medical diagnosis or treatment. If you have an urgent medical problem, call 911 immediately or contact your healthcare provider.
Human Papilloma Virus
How Is HPV Spread?
HPV is passed through skin-to-skin contact during vaginal, anal, or oral sex. Because the virus can be on skin not covered by condoms or barriers, it can sometimes be transmitted even when using protection—though condoms and dental dams still significantly lower the risk.
It can take weeks, months, or even years after exposure for symptoms to appear. Some people never develop symptoms at all, but can still pass HPV to others.
What Do Genital Warts Look Like?
Genital warts may:
- Appear as small, flesh-colored or gray bumps
- Be flat, raised, or cauliflower-like in appearance
- Show up on the vulva, vagina, cervix, penis, scrotum, anus, or thighs
- Sometimes itch or cause mild discomfort, but are often painless
Not all HPV types cause warts, and not all abnormal Pap results are caused by high-risk HPV.
Symptoms of HPV
Many people never know they have HPV. When symptoms do occur, they may include:
- Visible genital warts
- Itching, burning, or mild irritation in the genital area
- Abnormal Pap smear results (caused by changes in cervical cells)
Testing and Follow-Up
- Pap tests and HPV tests can detect cell changes or the presence of high-risk HPV types.
- If results are abnormal, your provider may recommend a colposcopy (a closer exam of the cervix) or a biopsy.
- Regular screening is key to catching changes early, when they are most treatable.
Treatment
There is no cure for HPV itself, but treatments can manage symptoms and reduce complications:
- Prescription creams or solutions for external genital warts
- In-office procedures like cryotherapy (freezing), cauterization (burning), laser, or surgical removal
- Regular Pap and HPV testing to monitor and treat abnormal cells if needed
In many cases, the body clears the virus naturally within 1–2 years.
Protecting Yourself and Partners
Taking steps to protect your sexual health can reduce your risk of HPV and its complications:
- Use condoms, internal condoms, or dental dams with every sexual encounter.
- Talk openly with partners about STI testing and history.
- Get regular Pap tests and HPV screenings as recommended.
- Support your immune system with rest, nutrition, exercise, and stress management.
HPV Vaccine at the Emma Goldman Clinic
The HPV vaccine (Gardasil 9) is available at the Emma Goldman Clinic. The vaccine protects against the HPV types most often linked to cervical, anal, throat, and other cancers, as well as those that cause most cases of genital warts.
- Recommended for all people of all genders starting at age 11–12, but can be given as early as age 9.
- Catch-up vaccination is available up to age 26, and in some cases may be considered up to age 45.
- The vaccine is safe, highly effective, and one of the best tools we have to prevent HPV-related cancers and warts.
Ask us about getting the HPV vaccine during your next visit.
HIV
What Is AIDS?
AIDS stands for Autoimmune Deficiency Syndrome. The following are symptoms seen with AIDS:
- Repeat vaginal yeast infections
- Irregular menstrual periods
- Abnormal Pap Smears
- Thick white coating or patches in the mouth or on the tongue (yeast)
- Rapid weight loss (15 or more pounds in 2 months if not due to diet or exercise)
- Cough with shortness of breath that continues to get worse
- Diarrhea
- Fever
- Night sweats
- Extreme tiredness
- Swollen glands in neck, armpits, or groin
- Pink or purple marks or bumps on the skin or inside your mouth
- These symptoms are common with many less serious diseases so talk to your health practitioner, especially if you have:
- More than one symptom at a time
- Any one symptom that lasts over 1 month
How Is HIV Passed From One Person To Another?
The virus is passed to other people through sexual contacts. This means exchange of vaginal secretions and seminal fluid. This includes putting the penis into the vagina and rectum. It also includes contact between genitals by mouth or through the use of sex toys.
The virus is also passed in the blood through sharing needles during intravenous drug use ("shooting up").
- Studies show that HIV cannot be transmitted by casual contact such as:
- Shaking hands, hugging, dry kissing (with no exchange of saliva), sneezing, or coughing
- Swimming in a pool with a person who is HIV infected
- Sharing eating and drinking utensils
- Sharing toilets, bathrooms, or kitchens
Who Is At Risk For Getting AIDS/HIV?
Anyone is at risk unless they are having sex with only one partner and that partner does not have any other partners. If either has had one or more other partners, they should have the HIV test. You are also more likely to be at risk if:
- You have sex without using condoms
- You share drug needles
- You have sex with gay or bisexual men
What Are The Tests For HIV?
There are two tests for HIV, the blood test and Orasure. With Orasure, a pad is placed in the mouth for 2 minutes. Both tests are sent to a laboratory for a reading. It itakes 7 to 10 days for results to come back.
There are very rarely false positive and false negative tests. If you are indoubt about the results, get tested again.
What Are The treatments for HIV?
Use Safer Sex practices:
- Always use a condoms with every sex act. (vaginal or rectal. also oral sex)
- Use a water-based spermicide as a lubricant for vaginal or anal sex.
- Decrease chance of eschanging body fluids (vaginal secretions, seminal fluid, and blood) by using other ways to express caring such as cuddling, touching, fantasizing, or mutual masturbation.
24 hour toll-free AIDS Hotline: 1 800-445-AIDS
Remember, AIDS has the potential for lasting longer than your partner!
The health information provided on emmagoldman.com is not intended or implied to be a substitute for professional medical advice. Nothing stated by this website or linked pages should be used for medical diagnosis or treatment. If you have an urgent medical problem call 911 immediately or contact your healthcare provider.
Hepatitis B
Symptoms
Some people never develop symptoms, while others may have mild to severe illness. When symptoms occur, they may include:
- Nausea or vomiting
- Stomach pain or loss of appetite
- Headache or fever
- Fatigue
- Yellowing of the skin or eyes (jaundice)
- Dark urine
- Liver tenderness or pain under the ribs
Symptoms may appear 1–4 months after exposure. Some people may carry the virus without symptoms but can still transmit it to others.
Treatment
There is no cure for hepatitis B, but treatment focuses on:
- Rest, hydration, and supportive care for short-term infections
- Antiviral medications for people with chronic hepatitis B to slow disease progression and reduce complications
- Regular monitoring of liver health
The most effective protection is vaccination, which is given as a series of shots. The hepatitis B vaccine provides long-lasting immunity and is strongly recommended for all infants, children, and unvaccinated adults at risk.
If Untreated
If left untreated, hepatitis B can cause long-term liver problems, including:
- Chronic hepatitis (ongoing infection)
- Cirrhosis (scarring of the liver)
- Liver failure
- Increased risk of liver cancer
- In rare cases, death
Protecting Yourself and Others
Taking steps to protect your health helps reduce the risk of HBV:
- Get the hepatitis B vaccine (available at the Emma Goldman Clinic).
- Use condoms or other barriers during sex to lower the chance of exposure.
- Avoid sharing needles, razors, toothbrushes, or other items that may come in contact with blood.
- If pregnant, ask your provider about hepatitis B testing and steps to prevent passing the virus to your baby.
⚠️ Medical Disclaimer
The health information provided on emmagoldman.com is for educational purposes only and is not intended as a substitute for professional medical advice. Nothing on this website or linked pages should be used for medical diagnosis or treatment. If you have an urgent medical problem, call 911 immediately or contact your healthcare provider.
Trichomoniasis
How Do You Get It?
Trich is spread primarily through sexual contact, including vaginal, anal, or oral sex. Transmission through shared wet items like towels or bathing suits is possible but very rare.
Symptoms
Many people with trich do not have symptoms. When symptoms do occur, they may include:
- For people with a vagina: frothy, yellow-green or gray discharge with a strong odor, vaginal itching or burning, soreness, redness, or pain during urination or sex.
- For people with a penis: burning after urination or ejaculation, discharge from the urethra, or irritation inside the penis.
- For anyone: genital discomfort or inflammation.
Because symptoms can overlap with other infections, it’s important to get tested for an accurate diagnosis.
Diagnosis
A healthcare provider can test for trich by examining a sample of vaginal or urethral discharge under a microscope or by using lab-based tests that detect the parasite more accurately.
Treatment
Trich is treatable and curable with prescription antibiotics such as metronidazole (Flagyl) or tinidazole.
Important reminders:
- Avoid alcohol while taking these medications, as it can cause severe nausea and vomiting.
- All sexual partners should be treated at the same time to prevent reinfection.
- Avoid sexual contact until you and your partner(s) have completed treatment and symptoms are gone.
If Untreated
If left untreated, trich can cause ongoing discomfort and increase the risk of:
- Pelvic inflammatory disease (PID) in people with a uterus
- Prostate inflammation in people with a penis
- Higher risk of acquiring or transmitting HIV and other STIs
Protecting Yourself and Partners
Taking steps to protect your sexual health reduces your risk of trich and other STIs:
- Use condoms or other barriers (such as internal condoms or dental dams) every time you have sex.
- Get tested regularly if you are sexually active, especially with new or multiple partners.
- Talk openly with partners about STI testing and treatment.
- Avoid sharing wet towels, washcloths, or swimsuits.
⚠️ Medical Disclaimer
The health information provided on emmagoldman.com is for educational purposes only and is not intended as a substitute for professional medical advice. Nothing on this website or linked pages should be used for medical diagnosis or treatment. If you have an urgent medical problem, call 911 immediately or contact your healthcare provider.
Pubic Lice (Crabs)
Symptoms
- Itching (from mild irritation to severe discomfort)
- Visible nits (eggs) attached to hair shafts
- Adult lice visible on hair or skin
- Irritation or small red bumps in the affected area
Diagnosis
Lice are diagnosed either through visual identification of live lice or by spotting their eggs (nits). Itching plus evidence of lice or nits usually confirms infestation.
Treatment
Pubic lice are treatable with over-the-counter lice medications, available as shampoos, lotions, or cream rinses. Generics are widely available—ask your pharmacist if you’re unsure which product to use.
- Apply treatment to all areas with coarse body hair (not just the pubic area).
- Leave on for the directed time, then rinse thoroughly.
- Repeat treatment in 7–10 days to kill any newly hatched lice.
General measures:
- Wash clothing, bedding, and towels in hot water and dry on high heat.
- Items that can’t be washed may be sealed in a plastic bag for 2 weeks or dry-cleaned.
- Clean or replace combs and brushes.
- Avoid close contact until treatment is completed.
- Recent sexual partners and close contacts should also be treated to prevent reinfestation.
Survival of Lice
- Head and body lice can survive 7–10 days off a human host.
- Pubic lice survive about 1–2 days off the body.
- Nits (eggs) hatch in 5–10 days, which is why repeat treatment is necessary.
⚠️ Medical Disclaimer
The health information provided on emmagoldman.com is for educational purposes only and is not intended as a substitute for professional medical advice. Nothing on this website or linked pages should be used for medical diagnosis or treatment. If you have an urgent medical problem, call 911 immediately or contact your healthcare provider.
Vaginal Imbalances
Some of the most common vaginal imbalances include:
- Yeast infections – often cause itching, irritation, and a thick, white discharge.
- Bacterial Vaginosis (BV) – usually causes a thin, gray or white discharge and a “fishy” odor, especially after sex.
- pH imbalances – can make the vagina more prone to infections or irritation.
Vaginal imbalances are not always sexually transmitted and are not a reflection of hygiene. They are simply a sign that your body’s natural environment has shifted. Many imbalances are easily treated with medication or lifestyle adjustments.
If you notice persistent odor, discharge, itching, burning, or discomfort, scheduling an exam or test is the best way to find out what’s going on and get relief.
Dental Dams and Oral Sex
What Is a Dental Dam?
A dental dam is a thin sheet of latex or polyurethane that creates a barrier between the mouth and the vagina or anus during oral sex. Dental dams help reduce the risk of transmitting or acquiring STIs.
👉 Dental dams are available at the Emma Goldman Clinic. Ask about them at your next visit.
How to Use a Dental Dam
- Place the dental dam flat over the vulva/vagina or anus before oral contact.
- Hold the dam in place during use.
- Do not flip it over—keep the same side against your partner’s body throughout.
- Use a new dental dam each time and for each area (never reuse).
Making Your Own Dental Dam
If dental dams are hard to find, you can make one from a condom or a latex glove.
From a condom:
- Unroll the condom completely.
- Use scissors to cut off the tip and the thick ring at the base.
- Cut lengthwise along one side to create a rectangle of latex.
- Place the sheet over the vulva or anus for protection.
From a glove:
- Cut off the fingers.
- Cut down one side to create a flat sheet.
- Place the sheet over the area you want to cover.
Like condoms, dental dams are for single use only—dispose of them after use.
⚠️ Medical Disclaimer
The health information provided on emmagoldman.com is for educational purposes only and is not intended as a substitute for professional medical advice. Nothing on this website or linked pages should be used for medical diagnosis or treatment. If you have an urgent medical
Add a drop of water-based or silicone lubricant on the side facing the body for more sensation.



Pelvic Inflammatory Disease
Why It Matters
Each recurrent episode of PID increases the risk of infertility, chronic pelvic pain, or ectopic pregnancy. Scarring of the fallopian tubes from repeated infections is the primary cause of PID-related infertility.
- Risk of infertility after PID episodes:
- 1st episode → ~11%
- 2nd episode → ~23%
- 3rd episode → ~54%
- 1st episode → ~11%
- If cervical gonorrhea is left untreated: up to 40% of cases may lead to PID.
- If treated adequately: risk of PID from cervical gonorrhea is near 0%.
Risk Factors
While anyone with a uterus can develop PID, risk is higher if you:
- Have an untreated STI (especially chlamydia or gonorrhea)
- Have multiple sexual partners, or a partner who has other partners
- Have a personal or family history of PID
- Recently had an IUD inserted (risk is slightly increased in the first few weeks after insertion, but IUDs remain a safe and effective contraceptive choice overall)
- Are in the first few days of your menstrual cycle (when the cervix is slightly more open)
Symptoms
PID may cause:
- Pelvic or lower abdominal pain
- Pain during sex
- Unusual vaginal discharge
- Irregular bleeding between periods or after sex
- Fever, chills, or nausea
- Painful or frequent urination
Sometimes PID has few or no symptoms, which is why regular STI screening is so important.
Diagnosis and Treatment
A healthcare provider can diagnose PID with an exam, lab tests, or imaging.
Treatment usually includes:
- Antibiotics (often a combination to cover multiple bacteria)
- Rest and follow-up appointments to confirm the infection is cleared
- Treating all sexual partners to prevent reinfection
Severe cases may require hospitalization. Prompt treatment is critical to prevent long-term complications.
Protecting Yourself and Partners
You can reduce your risk of PID by:
- Getting tested regularly for STIs if you are sexually active
- Taking steps to protect your sexual health (using condoms, dental dams, or other barriers)
- Talking openly with partners about STI testing and treatment
- Seeking treatment right away if you experience symptoms of an STI or PID
⚠️ Medical Disclaimer
The health information provided on emmagoldman.com is for educational purposes only and is not intended as a substitute for professional medical advice. Nothing on this website or linked pages should be used for medical diagnosis or treatment. If you have an urgent medical problem, call 911 immediately or contact your healthcare provider.






